Some health conditions are tough to talk about, and Persistent Genital Arousal Disorder (PGAD) is one of them. It’s a condition that flies under the radar, yet for those who experience it, the impact can be overwhelming. While it’s often associated with women, men can suffer from PGAD too — and the experience is just as distressing.
If you’ve ever wondered why these persistent sensations happen and what can be done about them, you’re not alone. Let’s tackle some common questions about PGAD in men, its causes, and how physical therapy can offer relief.
What Is Persistent Genital Arousal Disorder (PGAD) in Men?
PGAD is a condition where men experience persistent and unwanted feelings of genital arousal. This isn’t the same as sexual desire or excitement. In fact, these sensations often arise without any sexual thoughts or stimulation and don’t go away with orgasm. Imagine feeling aroused all the time — even during meetings, while driving, or trying to sleep. It’s uncomfortable, exhausting, and can take a real toll on mental health.
The prevalence of PGAD is still being studied, with research aiming to understand how widespread this disorder is among different populations. Studies investigate its occurrence and features to provide insights into its epidemiological and clinical aspects.
Various conceptualizations, potential origins, and impacts of PGAD are being explored to understand the underlying mechanisms and implications for treatment and patient care.
Definition and Overview
Understanding PGAD
Prevalence and Potential Causes of PGAD in Men
The exact cause of PGAD remains unclear, but several factors may contribute:
- Pelvic floor dysfunction: Overactive or tight pelvic floor muscles can exert pressure on nerves, leading to unwanted sensations.
- Nerve-related issues: Irritation or compression of the pudendal nerve, which supplies sensation to the genital area, might play a role.
- Pertinent peripheral nerves: Specific nerve pathways, such as the pudendal nerve, may contribute to the symptoms and experiences associated with PGAD.
- Psychological factors: Stress, anxiety, and other mental health conditions have been associated with PGAD, though it’s unclear if they are the causes or effects of the disorder.
- Medications: Certain medications, especially those affecting the nervous system, may trigger or exacerbate PGAD symptoms.
- Underlying medical conditions: Conditions such as prostatitis or spinal cord issues have been linked to PGAD.
PGAD Symptoms and Significant Distress
While each individual’s experience may vary, common symptoms include:
- Persistent genital sensations such as tingling, throbbing, or burning. The labia can also experience heightened tension and discomfort.
- Spontaneous erections that aren’t linked to sexual arousal.
- Sensations that don’t subside after orgasm.
- Physical discomfort or pain in the pelvic region.
- Emotional distress, anxiety, and sleep disturbances.
The Role of Stress and Anxiety
Stress and anxiety can exacerbate PGAD symptoms. These factors may lead to increased muscle tension and heightened nerve sensitivity, intensifying the sensations associated with PGAD. It is important to recognize the vital role of distress in the diagnostic criteria for PGAD, as it helps in distinguishing it from other conditions.
Differentiating PGAD from Similar Conditions: Pertinent Peripheral Nerves
It’s essential to distinguish PGAD from other conditions:
- Hypersexuality: Characterized by excessive sexual thoughts and behaviors, whereas PGAD involves unwanted physical sensations without accompanying desire.
- Priapism: A condition involving prolonged, often painful erections. In contrast, PGAD involves persistent arousal sensations without necessarily having prolonged erections.
Pudendal Nerve’s Role in PGAD
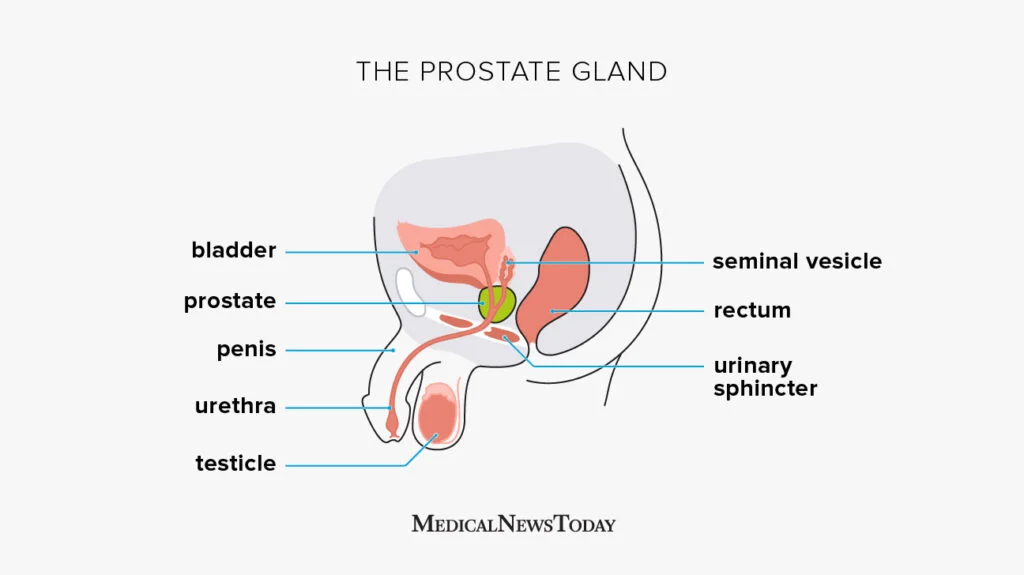
The pudendal nerve is a critical component of the peripheral nervous system, responsible for transmitting sensory information from the genital region to the spinal cord segments S2–S4. This nerve’s dorsal branch innervates the penis in males, playing a pivotal role in genital sensation.
Pudendal Nerve Entrapment and PGAD
Entrapment or irritation of the pudendal nerve, particularly its dorsal branch, has been implicated in the development of PGAD. Such nerve compression can lead to persistent, unwanted genital sensations characteristic of the disorder. This hypothesis is supported by clinical observations where decompression of the dorsal branch resulted in significant relief of PGAD symptoms.
Physical Therapy Interventions
Pelvic floor physical therapy offers several strategies to manage PGAD:
- Muscle relaxation: Manual therapy techniques aim to release tension in overactive pelvic muscles.
- Nerve desensitization: Nerve gliding exercises and gentle stretching can help reduce nerve irritation.
- Biofeedback: This technique helps retrain the pelvic floor muscles, promoting better coordination and relaxation.
- Relaxation techniques: Incorporating diaphragmatic breathing and mindfulness practices can help manage stress and reduce symptom severity.
Diagnostic Approach
Diagnosing Persistent Genital Arousal Disorder typically involves:
- Comprehensive medical history: Assessing symptoms, medical background, and potential contributing factors.
- Pelvic floor examination: Evaluating muscle tone, identifying trigger points, and assessing nerve sensitivity.
- Exclusion of other conditions: Ruling out disorders such as priapism or hypersexuality to ensure an accurate diagnosis.
Treatment Modalities
Effective management of PGAD often requires a multidisciplinary approach:
- Pelvic floor physical therapy: Targeted exercises and manual therapies to address muscle and nerve dysfunction.
- Medications: Prescription of nerve pain medications, muscle relaxants, or antidepressants to alleviate symptoms.
- Psychological support: Counseling or therapy to manage associated anxiety, stress, or depression.
- Lifestyle modifications: Implementing stress management techniques, engaging in regular physical activity, and identifying and avoiding individual triggers.
Impact on Daily Life
PGAD can significantly affect daily activities, leading to challenges such as:
- Emotional distress: Feelings of frustration, embarrassment, or isolation due to persistent symptoms.
- Sleep disturbances: Difficulty achieving restful sleep because of ongoing discomfort.
- Social withdrawal: Avoidance of social interactions or activities due to fear of symptom flare-ups.
Lifestyle Recommendations
To help manage PGAD symptoms:
- Practice mindfulness and relaxation: Engage in activities that promote relaxation and reduce stress.
- Maintain regular physical activity: Exercise can improve overall well-being and may help alleviate symptoms.
- Limit prolonged sitting: Taking regular breaks to stand or move can reduce pelvic pressure.
Prognosis and Hope
While there is no definitive cure for PGAD, many individuals experience significant relief through a combination of therapies and lifestyle changes. Collaborating with healthcare professionals, including pelvic floor physical therapists, can lead to improved symptom management and an enhanced quality of life.
Clinical Assessment and Diagnosis
Treatment and Management
Managing Persistent Genital Arousal Disorder (PGAD) involves a holistic and multidisciplinary approach that addresses both the physical and psychological aspects of the condition. The primary goal is to alleviate symptoms, improve quality of life, and enhance overall well-being. Researchers are encouraged to explore the influence of personality traits on the conscious suppression of PGAD symptoms, as further investigations in this area could yield critical insights into the condition.
Several treatment options are available for PGAD, including:
- Medications: Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are commonly prescribed to help manage the symptoms of PGAD. These medications can help regulate mood and reduce the intensity of unwanted arousal sensations.
- Pelvic floor physical therapy: A specialized physical therapist can assist in relaxing the pelvic floor muscles, improving blood flow, and reducing pain and discomfort. Techniques such as manual therapy, nerve desensitization, and biofeedback are often employed.
- Cognitive-behavioral therapy (CBT): This form of therapy helps patients identify and change negative thought patterns and behaviors that may be contributing to their symptoms. CBT can be particularly effective in managing the anxiety and stress associated with PGAD.
- Mindfulness-based therapies: Practices such as mindfulness-based stress reduction (MBSR) and mindfulness-based cognitive therapy (MBCT) can help reduce stress and anxiety, promoting overall well-being.
- Alternative therapies: Acupuncture, massage therapy, and other alternative treatments may provide additional relief and improve the quality of life for some patients.
Working closely with a healthcare provider to develop a personalized treatment plan is essential. This plan should be tailored to the patient’s unique needs and circumstances, ensuring the most effective management of PGAD symptoms.
The Role of Magnetic Resonance Imaging (MRI) in PGAD Research
Magnetic Resonance Imaging (MRI) plays a crucial role in PGAD research, particularly in identifying potential underlying causes of the condition. MRI can help detect anatomical abnormalities, such as sacral Tarlov cysts, which have been associated with PGAD. Additionally, functional MRI (fMRI) can be used to study brain activity and connectivity in individuals with PGAD, providing valuable insights into the neural mechanisms underlying the condition. Studies have shown that fMRI can help identify altered brain activity patterns in individuals with PGAD, particularly in regions involved in sexual arousal and emotion regulation. This advanced imaging technology is instrumental in advancing our understanding of PGAD and developing targeted treatment strategies.
Impact on Mental Health
The persistent and distressing nature of PGAD can have a profound impact on mental health. Men with PGAD often experience significant emotional distress, which can manifest as anxiety, depression, and a sense of hopelessness. The condition can also strain relationships, affect work performance, and disrupt daily activities, leading to feelings of isolation and loneliness.
Studies have shown that individuals with PGAD are more likely to experience:
- Anxiety: The constant and unwanted arousal sensations can lead to heightened anxiety, which in turn can exacerbate the symptoms of PGAD.
- Depression: The chronic nature of the condition can result in feelings of despair and hopelessness, further impacting the individual’s mental health.
- Trauma: The experience of PGAD can be traumatic, leading to feelings of shame, guilt, and self-blame.
- Relationship problems: The condition can create tension and frustration in relationships, leading to anger and resentment.
Addressing the mental health aspects of PGAD is crucial. Counseling, therapy, and support groups can provide much-needed help and support. Mental health professionals can assist patients in developing coping strategies, improving relationships, and enhancing overall well-being.
When using articles related to PGAD, it is important to consider the licensing requirements of a Creative Commons Attribution license. While certain uses are permitted, users must obtain permission from the copyright holder if their intended use exceeds what is allowed by law or the license.
Living with Persistent Genital Arousal Disorder
Living with PGAD can be challenging and distressing, affecting various aspects of daily life. Often experience intrusive and unwanted genital arousal that interferes with their lifestyle, causing anxiety, depression, and feelings of shame. These persistent symptoms can make it difficult to complete daily activities, maintain relationships, and experience pleasure during sex.
Individuals with PGAD need to seek help from healthcare professionals, including psychologists, pelvic floor physical therapists, and sex therapists, to develop coping strategies and manage symptoms. Support from a multidisciplinary team can provide the necessary tools to navigate the complexities of living with PGAD.
Managing Persistent Genital Arousal
Managing persistent genital arousal in PGAD requires a multidisciplinary approach, involving a team of healthcare professionals. Treatment options may include extensive psychotherapy, psycho-education, and pelvic floor physical therapy. Individuals with PGAD need to work with their healthcare team to develop a personalized treatment plan that addresses their unique needs and concerns.
How to Calm Down PGAD
Managing Persistent Genital Arousal Disorder (PGAD) involves a combination of strategies aimed at alleviating symptoms:
- Physical Interventions:
- Cold Therapy: Applying ice packs directly to the genital area can provide temporary relief from discomfort.
- Topical Anesthetics: Using numbing gels can help reduce sensations in the affected region.
- Lifestyle Modifications:
- Avoiding Tight Clothing: Wearing loose-fitting garments reduces unnecessary pressure on the genital area.
- Breaking Up Long Periods of Sitting: Taking regular breaks during extended periods of sitting can prevent symptom exacerbation.
- Stress Management: Practicing deep breathing and mindfulness techniques can help manage stress, which may trigger or worsen symptoms.
- Medical Interventions:
- Medications: Certain medications, such as muscle relaxants or nerve pain medications, may be prescribed to alleviate symptoms.
- Pelvic Floor Physical Therapy: Working with a specialized physical therapist can address muscle dysfunction contributing to PGAD.
Does PGAD Ever Go Away?
The duration of PGAD varies among individuals. Some may experience spontaneous remission, while others might have persistent symptoms. Effective management through a combination of therapies can lead to significant improvement, though a definitive cure remains elusive.
What Are the 5 Levels of Arousal in Men?
The human sexual response cycle comprises four phases:
- Desire: The initial phase involving sexual interest or libido.
- Arousal (Excitement): Characterized by physiological changes such as increased heart rate and erection in men.
- Plateau: A sustained period of sexual excitement before orgasm.
- Orgasm: The peak of sexual pleasure accompanied by ejaculation in men.
- Resolution: The phase where the body returns to its pre-arousal state.
These stages are consistent across genders, though individual experiences may vary. Understanding these aspects and the sexual response cycle can aid in recognizing symptoms and seeking appropriate interventions.
What Age Does PGAD Start?
PGAD can manifest at any age, affecting both men and women. Documented cases range from individuals in their 20s to those in their 70s. However, due to its rarity and the stigma associated with the condition, its exact prevalence, and typical onset age are not well-established.
Conclusion
Persistent Genital Arousal Disorder (PGAD) is a complex and multifaceted condition that requires a comprehensive and multidisciplinary approach to diagnosis and treatment. By addressing the physical, emotional, and psychological aspects of the condition, healthcare providers can help patients alleviate symptoms, improve quality of life, and enhance overall well-being. Continued research is essential to better understand the causes and mechanisms of PGAD and to develop more effective treatments and management strategies.
If you’re experiencing symptoms of Persistent Genital Arousal Disorder (PGAD) or other pelvic floor dysfunctions, seeking specialized care is crucial. At Pelvis NYC, Dr. Adam Gvili, a licensed Doctor of Physical Therapy, offers tailored treatment plans to address male pelvic health concerns in a comfortable and judgment-free environment.
Contact Information:
- Address: 110 West 17th Street, New York, NY 10011
- Phone: 929-590-3445
- Email: hello@pelvis.nyc
- Website: https://pelvis.nyc
For more details or to schedule an appointment, click this link.