What Is a Tight Pelvic Floor?
A tight pelvic floor happens when the pelvic floor muscles are overactive, shortened, or unable to relax fully. The pelvic floor is a group of muscles located in the pelvic region, supporting pelvic organs such as the bladder and rectum. Instead of supporting healthy bladder, bowel, and sexual function, these muscles stay “switched on,” leading to pain, tension, and dysfunction throughout the pelvis and core.
These muscles are also essential for bowel control, as well as bladder and sexual function. This condition is common—but frequently misunderstood. Many people are told to “do Kegels” when they actually need the opposite: relaxation, coordination, and targeted pelvic floor physical therapy.
Causes of Tight Pelvic Floor
Tight pelvic floor muscles can develop due to a mix of physical, behavioral, and emotional factors. Common causes include:
- Chronic stress: Ongoing stress keeps the pelvic floor, lower back, and inner thigh muscles tense, leading to persistent tightness and pelvic pain.
- Poor posture & weak core/thigh muscles: Surrounding muscles may not function properly, causing the pelvic floor to overcompensate and become tight.
- Habitual holding: Regularly holding in urine or bowel movements strains the pelvic floor and makes it harder to relax.
- Overactive pelvic floor (hypertonicity): Muscles that cannot contract and relax properly can cause spasms and increased tension.
- Weak pelvic floor muscles: Weakness can paradoxically cause tightness as the body keeps muscles engaged for support.
- Underlying health conditions: Pelvic organ prolapse, urinary incontinence, sexual dysfunction, and chronic pain disorders can all contribute to tight pelvic floor muscles.
Ways to address tight pelvic floor muscles:
- Diaphragmatic breathing & relaxation techniques to release tension
- Pelvic floor physical therapy: Manual therapy, stretching, and muscle retraining
- Strengthening core and thigh muscles while learning to properly contract and relax the pelvic floor
✅ Tip: Identifying the root cause and working with a pelvic floor physical therapist can reduce symptoms like pelvic pain, urinary issues, and erectile dysfunction.
Tight Pelvic Floor
A tight pelvic floor is not about weakness—it’s about too much muscle activity at the wrong time. The pelvic floor should contract and relax dynamically. When it cannot let go, symptoms develop. Other symptoms of a tight pelvic floor include chronic pelvic pain, painful sex, urinary urgency, constipation, and lower back pain.
According to research published in The Journal of Women’s Health Physical Therapy, overactive pelvic floor dysfunction is present in a significant percentage of patients with chronic pelvic pain, urinary urgency, and sexual pain disorders.
This issue affects all genders and ages, including athletes, postpartum individuals, desk workers, and people under chronic stress.
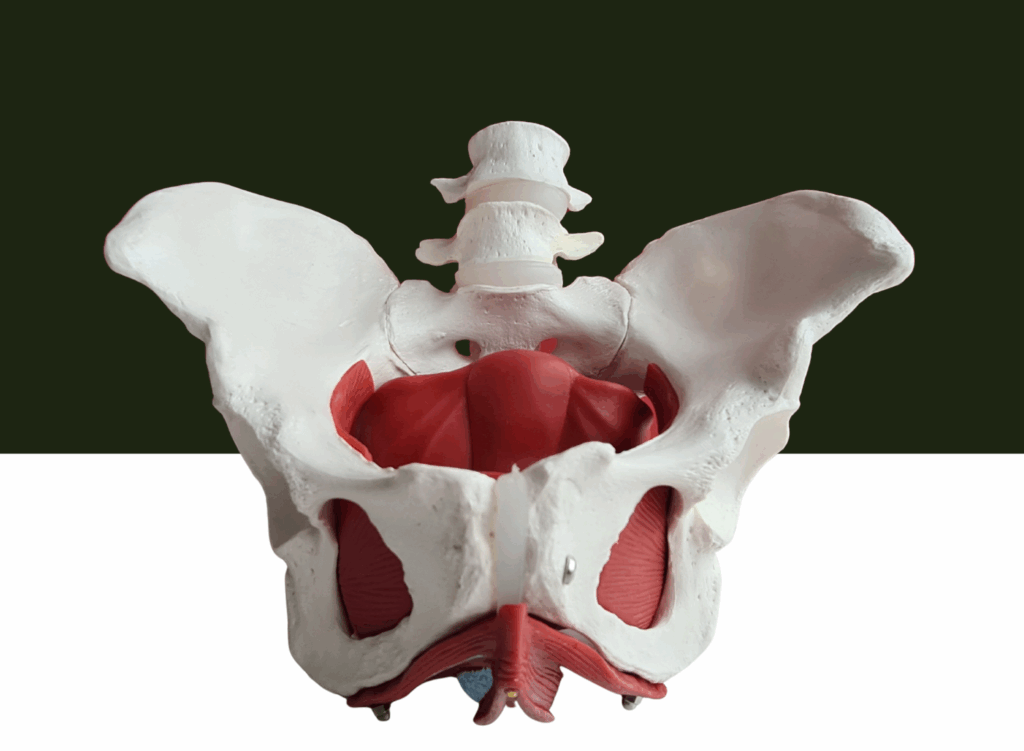
Pelvic Floor Muscles
The pelvic floor muscles form a sling at the base of the pelvis. The pelvic floor is made up of several pelvic muscles, including the perineal muscles, which stretch from the pubic bone at the front to the sitting bones and tailbone at the back. They support:
- The bladder and urethra
- The rectum and anal sphincter
- Sexual organs
- Core stability and posture
Healthy pelvic floor muscles can contract, relax, and lengthen. Pelvic floor muscles work in coordination with the diaphragm and core muscles to support pelvic organs and maintain pelvic health. Problems arise when they lose this flexibility.
When these muscles stay tight:
- Blood flow decreases
- Nerves become irritated
- Coordination with breathing and the core is disrupted
Pelvic Floor Physical Therapy

Pelvic floor physical therapy is the gold-standard treatment for tight pelvic floor dysfunction. Unlike general physical therapy, it focuses on the neuromuscular system of the pelvis.
A pelvic floor physical therapist may use:
- Internal and external myofascial release
- Breathing retraining
- Postural correction
- Nervous system down-regulation
- Movement re-education
At Pelvis NYC, treatment plans are individualized and trauma-informed, focusing on restoring function—not just reducing symptoms.
Tight Pelvic
The term tight pelvic is often used by patients to describe a cluster of symptoms rather than a single diagnosis. Some may also refer to this as a tense pelvic floor, which can result from stress, muscle imbalances, or chronic tension.
Common complaints include:
- Difficulty starting or fully emptying urine
- Pain with sitting or exercise
- Hip, low back, or tailbone pain
- Pain during or after sex
- Additional symptoms of a tense pelvic floor may include pelvic pain, lower back pain, hip pain, pain with urination, and difficulty starting a bowel movement.
Importantly, imaging tests often appear “normal,” which can delay proper diagnosis.
Erectile Dysfunction ED
A lesser-known contributor to erectile dysfunction (ED) is pelvic floor muscle tension.
In men, an overactive pelvic floor can:
- Restrict blood flow to the penis
- Compress nerves involved in arousal
- Interfere with ejaculation
Painful ejaculation is the most common sexual problem for men with a tight pelvic floor, occurring in an estimated 39-58% of men with chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS).
Kegel exercises are often recommended to strengthen pelvic floor muscles and improve sexual health, but should be used with caution in cases of muscle tension.
Studies in The British Journal of Urology International show that targeted pelvic floor physical therapy can significantly improve erectile function—especially when ED is not primarily vascular.
Pelvic Pain
Pelvic pain related to a tight pelvic floor can be sharp, aching, burning, or pressure-like. It may be constant or activity-dependent.
Common diagnoses linked to pelvic floor tension include:
- Vulvodynia
- Chronic prostatitis / CPPS
- Interstitial cystitis
- Endometriosis-related pain
- Pudendal neuralgia
Pain is not “all in your head.” Muscle tension and nervous system sensitization are real, measurable contributors.
Tight Pelvic Floor Muscles
Tight pelvic floor muscles often coexist with:
- Jaw clenching
- Shoulder tension
- Shallow chest breathing
This pattern reflects a global stress response. Tense muscles throughout the body, including the pelvic floor, are often linked to chronic stress and anxiety, which can contribute to hypertonic pelvic floor muscles. The body learns to brace instead of release.
Key insight:
Tight muscles are often overworked, not strong.
Strengthening without relaxation can worsen symptoms.
Overactive Pelvic Floor Muscles
Overactive pelvic floor muscles fire when they shouldn’t—during urination, bowel movements, or penetration.
Symptoms may include:
- Urinary urgency or frequency
- Constipation or incomplete bowel movements
- Bowel dysfunction, which may lead to chronic constipation and straining during bowel movements due to pelvic floor tension
- Pain with tampons or exams
- Pain after ejaculation
Clinical guidelines from the American Physical Therapy Association (APTA) recommend down-training and coordination before strengthening.
Overactive Pelvic Floor
An overactive pelvic floor is often driven by:
- Chronic stress or anxiety
- Past pelvic trauma or surgery
- High-impact sports
- Postural habits (constant core bracing)
This is why a whole-body approach matters. Treating only the pelvis ignores the root cause.
Pelvic Floor Problems
Pelvic floor problems exist on a spectrum. Tightness is one end; weakness is another. Many people fluctuate between both.
Misdiagnosis is common. For example:
- Someone with urgency may be told they have a “weak bladder”
- Someone with pain may be told tests are normal
A comprehensive pelvic floor exam changes everything.
Male Pelvic Floor
The male pelvic floor plays a crucial role in:
- Urinary control
- Sexual performance
- Core strength
Pelvic floor muscles play a crucial role in sexual health. Sexual dysfunction in females can manifest as pain during intercourse, while in males it may lead to erectile dysfunction or pain during ejaculation.
Men are less likely to be referred to pelvic floor therapy, despite strong evidence supporting its effectiveness for pelvic pain and ED.
At Pelvis NYC, male pelvic health is treated with the same depth and expertise as female care.
Pelvic Floor Muscle Function
Optimal pelvic floor muscle function includes:
- Full relaxation
- Timely contraction
- Endurance when needed
Muscle relaxation is essential for pelvic floor health, as it allows the muscles to release tension and function optimally. Diaphragmatic breathing can help lengthen pelvic floor muscles so they remain strong and flexible.
When relaxation is missing, function suffers—even if strength is present.
This is why “just doing Kegels” is not a universal solution.
Muscle Tension
Chronic muscle tension, especially from tense pelvic floor muscles, alters pain perception. Tight muscles send constant signals to the nervous system, reinforcing pain loops. Chronic pain from an overactive pelvic floor can have a devastating impact on an individual’s psychological wellbeing.
Pelvic floor physical therapy works by:
- Reducing muscle tone
- Improving tissue mobility
- Calming the nervous system
Over time, pain thresholds normalize.
Stretching Exercises
Targeted stretching exercises can support recovery—but only when prescribed correctly. Pelvic floor stretches and pelvic floor exercises, when performed correctly, can help relax and lengthen the muscles. Stretching exercises such as Happy Baby Pose and Child’s Pose are effective ways to relax pelvic floor muscles. Gentle movement and regular stretching can help relax tense pelvic floor muscles and ease discomfort. Relaxation exercises and relaxation techniques, such as deep belly breathing, yoga stretches like Child’s Pose, and mindfulness practices, are also helpful for managing a tight pelvic floor.
Helpful approaches often include:
- Diaphragmatic breathing
- Hip and pelvic mobility work
- Gentle lengthening, not forcing
Generic stretching routines from social media may aggravate symptoms if timing and technique are wrong.
When to Seek Help
You should consult a pelvic floor specialist if you experience:
- Persistent pelvic pain
- Urinary or bowel dysfunction without clear cause
- Sexual pain or dysfunction
- Symptoms that worsen with stress
For the best pelvic floor care, consider consulting a pelvic floor physical therapist. They can evaluate your symptoms and determine the right exercise therapy plan tailored to your needs.
Early intervention leads to faster recovery.
Why Choose Pelvis NYC?
Pelvis NYC specializes exclusively in pelvic floor physical therapy. Their clinicians have advanced training in complex pelvic pain, overactive pelvic floor disorders, and sexual health conditions.

Patients benefit from:
- One-on-one expert care
- Evidence-based techniques
- A supportive, judgment-free environment
👉 Book a consultation with Pelvis NYC to address tight pelvic floor symptoms at the source—not just manage them.
Frequently Asked Questions (FAQ)
What causes a tight pelvic floor?
Stress, trauma, posture, high-impact exercise, surgery, and chronic pain conditions are common contributors.
Can a tight pelvic floor go away on its own?
Mild cases may improve, but persistent symptoms usually require pelvic floor physical therapy.
Are Kegels bad for a tight pelvic floor?
Often yes. Strengthening without relaxation can worsen overactivity.
How long does pelvic floor physical therapy take?
Many patients notice improvement within 6–8 sessions, though complex cases may take longer.
Does a tight pelvic floor affect men and women differently?
Symptoms differ, but the underlying muscle dysfunction is similar.